Climate changes respiratory health

Climate change is impacting the air we breathe.
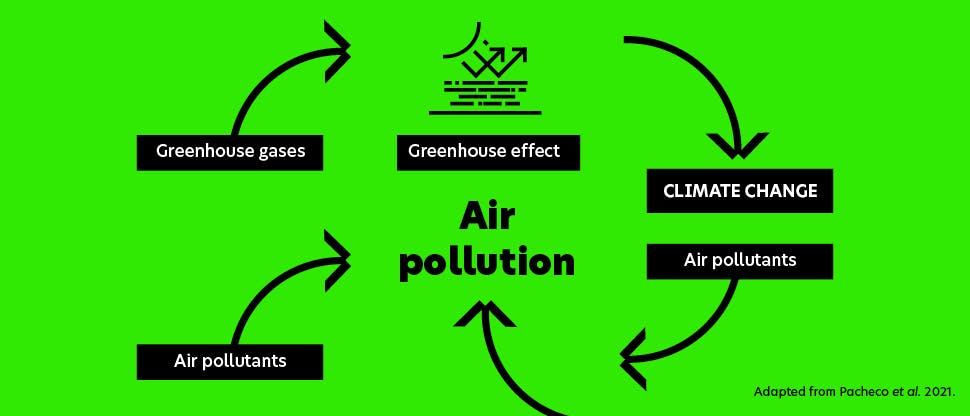
Burning fossil fuels, deforestation, livestock production and industrial processes are all examples of human activities which increase greenhouse gas emissions and drive climate change.1 As a result, hot extremes have become more frequent and more intense, with global surface increasing faster since 1970 than in any other 50-year period over at least the last 2000 years.2
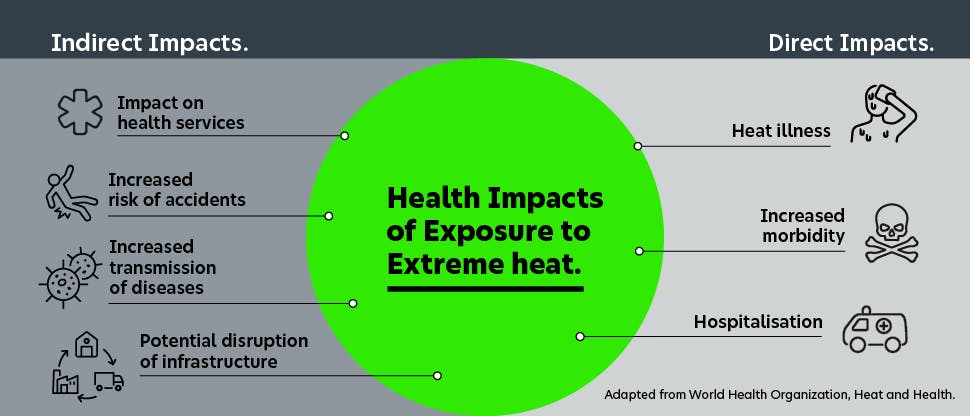
These extreme weather episodes pose a significant threat to health and life.1 Vulnerable groups, such as elderly individuals, pregnant women and children, people with disabilities, and those with chronic medical conditions are at the highest risk.1 Among its many devastating effects, climate change also impacts respiratory systems critical to human health.3
In this ever-changing world, patients will look to their primary healthcare providers to help them adapt. Healthcare professionals like you will be crucial in advising and supporting patients through these new challenges. And Haleon is here to support you. We’re committed to not only helping you understand this new health landscape, but to also support you as you help your patients navigate it too.
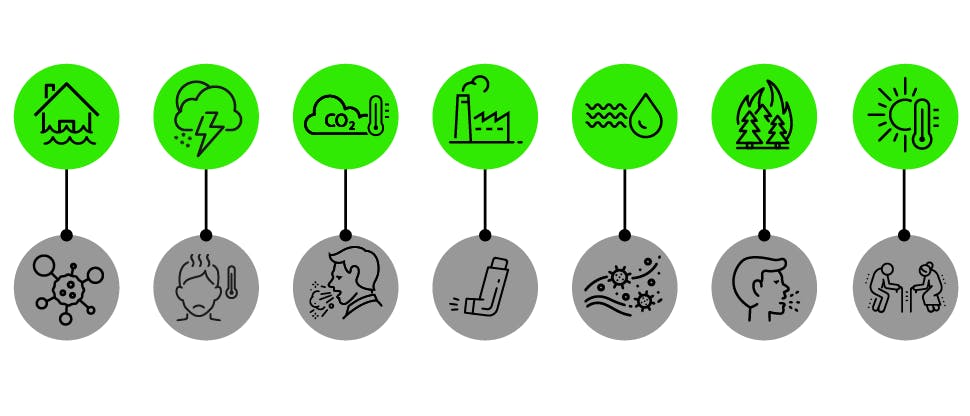
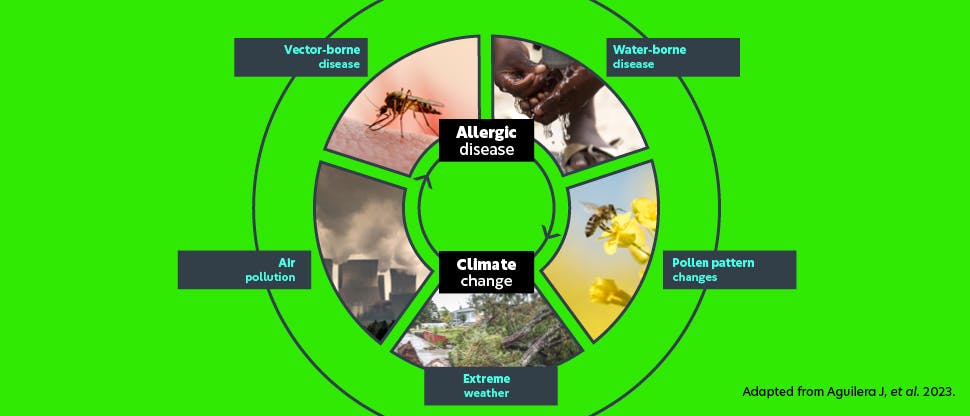
There is no single climate change event that impacts respiratory health.4-10
There are many facets to climate change and extreme weather, and their effects are felt across of wide spectrum of respiratory health conditions.4-10
These include:
- Flooding encourages mould growth which contributes to asthma, allergic rhinitis and sinusitis4
- Rapid weather changes have increased the risk of flu epidemics5
- Rising temperatures and CO2 levels contribute to allergy season arriving earlier and lasting longer6
- Air pollution and high temperature exacerbates asthmatic symptoms7
- Lower temperature and humidity create favourable conditions for flu transmission8
- Wildfire smoke contains microscopic particles which contribute to coughing and asthma flare-ups9
- Heat waves increase mortality, with the elderly being particular at risk10
Select a climate change event to learn how it impacts respiratory health
Read more



Cough
As our air quality changes with climate change, what does that mean for cough conditions?
Coming soon


Otri Allergy Products
Find out how our products can help your patients suffering from allergic rhinitis.