Managing gum disease in patients

Managing periodontal disease
Early to moderate periodontal disease can be successfully managed with ‘in chair’ treatments and supported by ‘at home’ care. Explore the different management approaches that have been shown to be effective.
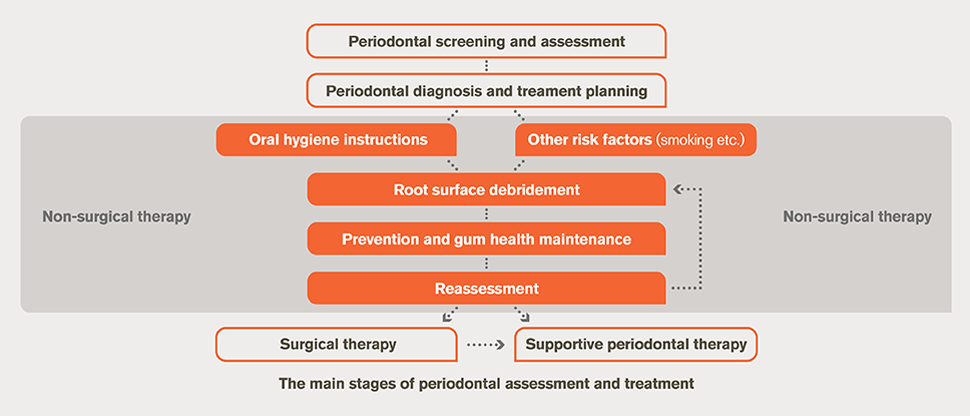
For most patients with early to moderate periodontal disease, non-surgical therapy is a highly effective form of gum disease management1
Non-surgical therapy should include:1
- Regularly advising and instructing your patients on how to maintain good oral hygiene
- Root surface debridement (electronic or hand scaling), ensuring regular removal of attached plaque biofilms and non-attached microflora in the gingival sulcus and periodontal pockets
- Elimination of plaque-retentive factors such as calculus and restoration overhangs
This can achieve:1
- Control of the bacteria and plaque challenge characteristic of gingivitis or periodontitis
- Resolution of local risk factors
- Minimisation of the effect of systemic risk factors
- Reduction of inflammation
- Improvement in overall periodontal health
Flow chart adapted from British Society of Periodontology, 20161
Daily effective plaque removal is as important to your patients’ gum health as tooth scaling and polishing1
Ensuring your patients have the right self-care regime is critical to preventing the development of gingivitis and reducing the risk of periodontitis.1

Daily care: Prevention and gum health maintenance
Regular advice for your patients’ daily care regime should include:1
- Twice-daily brushing1 with a specialist gum health toothpaste
- Manual or powered toothbrush with a small head and medium texture1
- Daily interdental plaque control between the teeth to below the gum line before brushing1
- Behavioural change methods for patients who struggle to keep to their daily care regime1

Intensive gum treatment
In patients with acute gingivitis, or when cleaning is difficult, short-term, intensive care should be recommended:
Gum disease treatments: helping your patients change their behaviour
In addition to regular professional cleans, preventing and managing periodontal disease both rely on the ability and proactivity of patients to remove plaque themselves. Maintaining gum hygiene may require patients to change their behaviour in terms of brushing, interdental cleaning and other oral hygiene techniques, in addition to lifestyle changes such as stopping tobacco use and improving nutrition.1,3
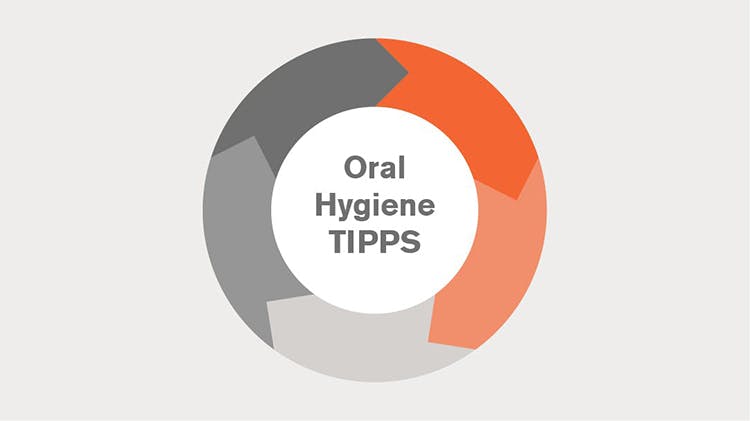
Oral hygiene tool: TIPPS1
Oral hygiene TIPPS is a tool based on behavioural theory that aims to make patients feel more confident in their ability to perform effective plaque removal. Developed by the Scottish Dental Clinical Effectiveness Programme, the intervention is as follows:3
- Talk with the patient about the causes of periodontal disease and discuss any barriers to effective plaque removal
- Instruct the patient on the best ways to perform effective plaque removal
- Ask the patient to practise cleaning his/her teeth and to use the interdental cleaning aids whilst in the dental surgery
- Put in place a plan which specifies how the patient will incorporate oral hygiene into daily life
- Provide support to the patient by following up at subsequent visits
TIPPS wheel adapted from the Scottish Dental Clinical Effectiveness Programme, 20143
Providing continuing periodontal support for optimum gum health management
Even with patients who regularly practise good oral hygiene, evidence has shown that potentially pathogenic bacterial flora can re-establish themselves 3 months after root surface debridement.1 This is why it’s recommended for patients with periodontitis to initially be recalled every 2–4 months,1 depending on their history. It also gives you a chance to provide continuing oral hygiene coaching.1

Taking a team approach to periodontal treatment and the role of the hygienist in gum disease management
A team approach from a dentist and hygienist can be a successful formula for periodontal management. However, good communication between both professionals, as well the patient, is critical to ensure the objectives of the treatment plan are realised. A simple periodontal proforma can be used by dentists and hygienists to ensure a clear structured plan, as well as to outline how the treatment objectives will be achieved.1
| Example periodontal team care proforma1 | |
| Diagnosis | Localised gingivitis |
| General prognosis | Good prognosis (with improved oral hygiene management at home and better diet) |
| Risk factors | Often only brushes once per day and diet high in junk food |
| Oral hygiene advice | Twice-daily brushing with electric toothbrush and interdental plaque control with dental tape |
| Preventative advice | Reduction in junk food and twice-daily use of gum health toothpaste |
| Debridement | Full mouth subgingival debride all probing depth ≥5mm with local anaesthesia |
| Reassessment | 3 months (oral hygiene), 6 months post-root surface debridement (to repeat periodontal charting) |

Referring patients with periodontal disease
General dental practitioners have a responsibility to screen, give diagnoses and institute treatment plans for periodontal disease. However, occasionally some cases may call for referral due to their extent and complexity.1
Factors to take into account when making a decision on whether to refer a patient with periodontal issues may include:1
- Disease severity and treatment complexity
- The patient’s desire for specialist care
- The knowledge, experience and training of the dental practitioner who is considering referral
- Factors that might complicate a management plan, such as a patient’s medical history or other comorbidity
Offering effective gum disease management to help your patients on their journey to optimal gum health
Causes and mechanisms
Find out about the causes and mechanisms behind periodontal disease.
Impact on patient quality of life
Find out about the impact periodontal disease has on patients’ daily lives.
