Allergic Rhinitis Causes & Mechanisms

The “allergic cascade” and its role in allergic rhinitis (AR)
The “allergic cascade” and its vital role in allergic rhinitis (AR)1
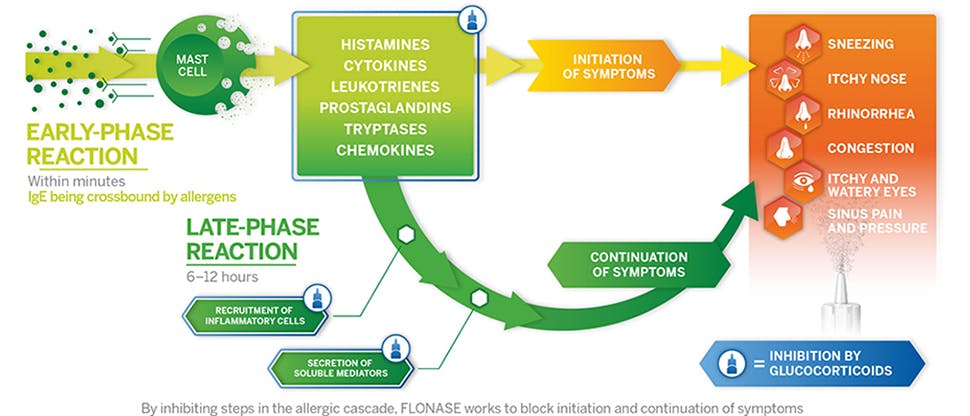
The body’s immune response to allergens includes a series of early- and late-phase reactions—the allergic cascade. There are several allergic mediators involved in this cascade, not histamines alone.3
Typically, the allergic cascade follows this pattern3:
- Exposure and sensitization to an allergen
- Early-phase response upon re-exposure to an allergen
- Late-phase response initiated by early-phase allergic mediators
When the body is exposed to an allergen:
- Sensitization involves being exposed to an allergen for the first time3
- The body produces immunoglobulin E (IgE) in response to the allergen, but an allergic reaction/symptoms does not yet occur3
- Re-exposure to an allergen triggers an early-phase response that typically occurs within minutes3
- IgE bound to receptors on mast cells bind to the allergen, crosslinking the IgE3
- When sufficient crosslinking occurs, the mast cells explode releasing histamine and many other inflammatory mediators, such as cytokines, leukotrienes, prostaglandins, eosinophils, and thromboxanes1,3
- The late-phase response occurs from 6-12 hours after allergen re-exposure1
- In this late-phase, immune cells, such as eosinophils, secrete substances that further promote the inflammatory response and recruit other immune cells into the reaction, perpetuating the inflammation and resulting symptoms1,3
- The symptoms can be more severe and persistent than those in the early phase1,3
The end result is the allergic response consisting of a range of bothersome symptoms, often impacting patient quality-of-life, such as rhinorrhea (runny nose), sneezing, congestion, and pruritus (itching).1
In fact, 71% of AR patients suffer from either moderate or severe allergy symptoms.4





